-
Mon - Sat
08:00am - 08:00pm
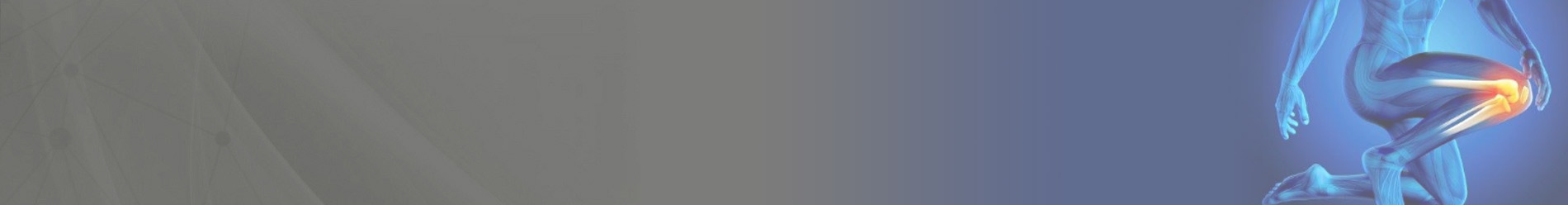
The knee joint is made up of three bones and four main ligaments. The knee is formed by the femur (the thigh bone), the tibia (the shin bone), and the patella (the kneecap). Several muscles and ligaments control the motion of the knee and protect it from damage at the same time. Two ligaments on either side of the knee, called the medial and lateral collateral ligaments, stabilize the knee from side-to-side.
The anterior cruciate ligament (ACL) is one of a pair of ligaments in the center of the knee joint that form a cross, and this is where the name “cruciate” comes from. There is both an anterior cruciate ligament (ACL) and a posterior cruciate ligament (PCL). Both of these ligaments function to stabilize the knee from front-to-back during normal and athletic activities. The ligaments of the knee make sure that the weight that is transmitted through the knee joint is centered within the joint minimizing the amount of wear and tear on the cartilage inside the knee.
The weight-bearing surfaces of your knees are covered with a layer of cartilage (called as”articular cartilage”). There are also two shock absorbers in your knee on either side of the joint between the cartilage surfaces of the femur and the tibia. These two structures are called the medial meniscus and the lateral meniscus. The menisci are horseshoe-shaped shock absorbers that help to both center the knee joint during activity and to minimize the amount of stress on the articular cartilage. The combination of the menisci and the surface cartilage in your knee produces a nearly frictionless gliding surface.

The main muscles that move the knee joint are the quadriceps and hamstring muscles. The quadriceps attaches to the patella, and the patellar tendon connects this muscle to the front of the tibia. When the quadricep muscles contract the knee extends. In contrast, when the hamstring muscles contract, they pull the knee into flexion.
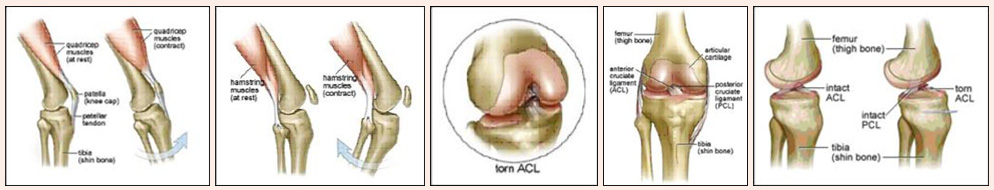
The anterior cruciate ligament (ACL) is one of a pair of ligaments in the center of the knee joint that form a cross, and this is where the name “cruciate” comes from. There are both an anterior and a posterior cruciate ligament (PCL). Both of these ligaments function to stabilize the knee.
In medical terms, the ACL is the primary restraint to anterior displacement of the tibia on the femur. This means that when the ACL is injured, the shinbone can slide forward on the thighbone, causing the knee to “give way”buckle and the patient complains of Instability.
Some people who rupture their ACL can recall the exact moment at which they felt it pop. This usually happens when changing direction quickly in pivoting or cutting sports like soccer, landing from a jump in sports such as basketball, or falling while skiing. Other than sports the common causes of ACL injury is fall of two wheelers in road traffic accident, dashboard injury, sudden twisting to knee by putting foot on uneven ground, pot hole or even falling from stairs.
The four “classic” symptoms that people may feel when they tear their ACL are:
Typically X-ray show no bony injury. If all or most of the above is true than one should seriously consider a ligament injury in the knee. Secondly other structures may also be injured along with ACL like meniscus (cartilage), other ligament like MCL, LCL, or PCL. Examining an athlete immediately after they have had a knee injury can sometimes be difficult and it is often not possible to tell what structures, if any, have been injured. A better examination can usually be obtained after the swelling has gone down and the pain from the injury has subsided. Although accurate diagnosis of the exact injury can be difficult, it is relatively certain that an athlete who develops a swollen knee immediately after an injury should not return to play and should seek medical evaluation.
ACL injuries appear to be happening more frequently today than they did in the past. This is in part because most athletes demand much more from themselves as compared to a generation ago. As the speed and agility of athletes increases, so does the amount of force that is sent through the ligaments of the knee. Women appear to be particularly susceptible to ACL injuries, and there is an ongoing debate in the sports medicine community about why this may be the case. In 1995, an article was published in the American Journal of Sports Medicine that found that female basketball players tore their ACL’s four times more often than male basketball players. While research have shown that the increased rate of ACL injuries in women may be due to differences in ligament strength, anatomy of the knee, jumping ability, muscle strength and coordination. As ACL injuries have become more common, more and more research is being done on how to prevent them.
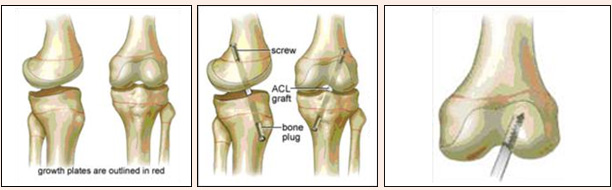
ACL injuries do occur in children. The child tears his or her ACL while playing sports or in an accident. The bones and joints of children are very different from the bones and joints of adults because children’s bones are still growing. This can make an ACL injury a bit more complicated for the children. The orthopaedic surgeon will want to find the best way to make sure that your child has a good knee that functions normally and does not hurt. This can be difficult because children are very active and it is hard to get them to slow down and avoid certain activities that may damage their knees. At the same time, ACL surgery for children is more difficult than it is in adults because there is the risk that the normal development of the bones can be changed by the surgery. There are some situations in which ACL injuries in children can cause enough looseness in the knee that participation in certain sports carries a very high risk of damaging the rest of the knee if the ACL is not fixed. These sports involve running, jumping, and changing direction quickly, like soccer, basketball, baseball, or skiing. In this situation, the child should either stop participating in these sports, or should get his/her ACL fixed. However, if the child does not play these sports, or if doctor believes that the child’s knee does not have a significant amount of looseness after the ACL has been torn, then the child may not need the surgery.
Currently, there are no solid recommendations for which surgical techniques are best for which age groups. Children who are close to maturity and generally more than about fourteen years old can have their ACL’s replaced safely with standard techniques. Children who are much younger may need to either wait until they are older, or if their knee is unstable enough they may need to have a different type of reconstruction that avoids drilling holes through the growth plate.
An ACL injury should be treated with a splint, ice, elevation of the limb, and pain relievers such as nonsteroidal anti-inflammatory drugs. The patient should not continue to play until evaluation and treatment has taken place. Some people may need crutches to walk until the swelling and pain has improved. Physical therapy may help regain joint motion and leg strength.
In the case of a serious knee injury, do not attempt to move the joint. A splint should be used to keep the knee straight until evaluation by trained medical personnel has been performed.
Do not return to play until proper evaluation and treatment has taken place.
Anyone with a serious knee injury should seek medical attention for x-rays and evaluation.
More important, if someone’s foot is cool and blue after a knee injury, they may have dislocated their knee and injured the blood vessels to the foot. This is a true medical emergency that requires immediate professional help.
Use proper techniques when playing sports or exercising. Several women’s collegiate sports programs have reduced ACL tears through a training program that teaches athletes how to minimize the stress they place on their ACL.
Although the issue is controversial, the use of knee braces during aggressive athletic activity, such as football, has not been shown to decrease the incidence of knee injuries and may give the player a false sense of security.
To diagnose a torn ACL, doctor at A+ Center first wants to know as much as possible about how the injury occurred. Be prepared to describe:
Doctor at A+ Center examines your knee to determine if the ACL is torn. Commonly used exams are the Lachman’s test and the pivot shift test.
If the movement in your knee is restricted by swelling or by contraction of the muscles in the back of your upper leg, doctor may not be able to detect a torn ACL with these tests.
ACL tears don’t show up on X-rays, although certain types of shin fractures associated with ACL tears may be visible. In diagnosing a torn ACL, some studies show that magnetic resonance imaging (MRI) has the same accuracy as a careful history and physical exam. Depending on the nature of the injury and other exam findings, however, an MRI is sometimes helpful in identifying damage to other structures in the knee treatment.
You and doctor at A+ Center may choose nonsurgical rehabilitation if:
Nonsurgical rehabilitation may also be appropriate for a child or an adolescent with a torn ACL. If your child has no damage to the knee other than to the ACL and can avoid high-risk activities, the doctor may recommend postponing surgery until your child’s bones have finished growing, although with current techniques, ACL reconstruction is generally possible without damaging the growth plate in growing children.
As with all treatment options, you’ll want to consider the trade-offs before deciding if nonsurgical rehabilitation is the best choice for you.
The goal of physical therapy is to strengthen the muscles around your knee to make up for the absence of an intact ACL. Training focuses on the:
Some exercises can be done at home. Others require the use of weight machines, exercise bicycles or treadmills, which may require visits to A+ Orthopedic & Sports Med Center. In the early stages of rehab, you work on re-establishing full range of motion in your knee. Then you progress to knee, hip and ankle-strengthening exercises combined with training to improve your stability and balance. Finally, you work on training specific to your sport or work activities, including exercises to help you prevent further injury, such as learning how to land properly from a jump.
A nonoperative rehabilitation program may be easier and less painful than the physical therapy needed after surgery. You can usually expect to be back to your normal daily activities within a month. However, physical therapy can be time-consuming, especially in the first few months after your ACL injury. To maintain maximum knee stability, your doctor will probably recommend lifelong strength and stability exercises for your legs.
You’ll need to change your activities to avoid high-risk sports that could further damage your knee. Avoid activities that include jumping, cutting, pivoting, and sudden slowing down or stopping (deceleration), such as basketball, football and soccer. You’ll likely be able to do other activities, such as jogging, swimming and bicycling, without difficulty. When paired with strength and stability exercises, activity modification reduces the risk of future knee problems. However, people who continue to participate in sports or activities that involve cutting, pivoting or sudden deceleration may find their knee “gives way.” Before you decide on a course of treatment, ask yourself if you’re willing to change your activities and give up those that may further damage your knee.
A knee brace doesn’t take the place of the torn ACL, but it can help stabilize your knee if you should choose nonoperative management while you take part in activities such as kabaddi, hockey, tennis or hiking over uneven ground. These braces are usually custom fitted or tailored.
With the aid of a brace, most people can continue to participate in many of their previous activities that don’t involve jumping, cutting and pivoting. People wearing knee braces report fewer episodes of instability or giving way, but it’s not known exactly why this occurs.
You may continue to experience instability in your knee during certain types of activities, even while wearing a brace. If this happens, consider making additional changes in your activities or reconsider surgical reconstruction. These repeated events could damage the cartilage and other parts of your knee.
If instability continues even after leg strength and knee motion has returned, most orthopedists will recommend a reconstruction of the ACL. The old ligament cannot be fixed, so a new one needs to be constructed. Usually a piece of the patellar tendon (the tendon connecting the kneecap to the tibia) is used, although the hamstrings can also be effective. Cadaveric grafts may also be used to reconstruct the ACL.
Surgical treatment involves reconstructing the ACL by replacing it with another tendon (graft) from your own body (autograft).
How do you prepare?
ACL surgery is done in a hospital or outpatient surgical clinic. The surgeon may recommend regional (epidural) anaesthetic, in which only your legs are numb, or a general anaesthetic, which affects your entire body and puts you in a temporary state of unconsciousness.
There are two graft options while reconstructing ACL
Some research has shown small differences in outcomes of patellar tendon grafts and hamstring grafts. Consider these pros and cons:
Type of graft Potential advantages Potential disadvantages. Patellar tendon graft Longer history of successful results More frontal knee pain. A greater number return to high-level activity, which may be preferable for serious athletes. Hamstring tendon graft Less frontal knee pain Residual hamstring weakness.
Not all research studies agree with these possible pros and cons. And with ever-improving surgical and rehabilitation techniques, these differences may become smaller still. Both grafts are about equal in regard to the number of people who return to their previous level of activity.
ACL surgery is usually done with arthroscopic techniques. An orthopedic & sports surgeon at A+ Center specialized in bone, muscle and joint surgery performs the procedure. The entire procedure takes two hours.

After ACL surgery your knee will be placed in a splint or brace for your comfort and protection. Most people go home on the day of surgery and use crutches for the first two to four weeks. This first week at home can be challenging because your mobility is restricted and your typical daily activities are more difficult. During this period you’re largely dependent on others, so it’s important that you have someone at home who can help.
It typically takes about six months of physical therapy and strengthening exercises before you’ll be able to return to your previous level of activity. You’ll need to do a lot of work that will take a significant amount of time. Before deciding to have surgery, make sure you’re motivated enough to complete the rehabilitation program.
Expect your rehabilitation to occur in roughly three phases. Progression from one phase of rehab to the next depends on the nature of your particular injury and how well you master the goals within each phase. Your rehab may be shorter or longer than this example:
Phase 1. The first phase of postoperative rehabilitation begins on the first day after surgery and takes about six to eight weeks. It consists of controlling the pain and swelling in the knee, regaining your range of motion, and preserving muscle strength. You work with a physical therapist a few times a week at first, then once every week or two as you progress. On days when you don’t have a therapy session, you exercise at home for 30 to 60 minutes a day.
Phase 2. The second phase of rehab typically lasts from two to four months after surgery. During this phase, you focus on controlling swelling and recovering full muscle strength. In addition to daily strengthening exercises, you begin stability and balance training. You see the physical therapist less often, but you continue with 30 to 60 minutes of exercises each day.
Some exercises require the use of weight machines, exercise bicycles or treadmills that you might do in a supervised clinic setting. Depending on the facilities available where you receive treatment, you may need to visit an athletic club or fitness center or A+ Center to do some of the exercises.
Phase 3. The final phase of postoperative rehab lasts several months after surgery and consists of a gradual return to full activity. This requires full motion, normal muscle strength and the absence of swelling. You’ll continue with stability, balance and strength training as well as training specific to your sport or work activities. This may include exercises to help you prevent further injury, such as learning how to land properly from a jump.
After ligament reconstruction and rehabilitation, you should be able to return to full activity without a brace. It’s important not to try to return to full activity too soon because your knee may become inflamed or re-injured. The graft needs to heal, and too much stress before it’s completely healed may increase the risk of the graft failing.